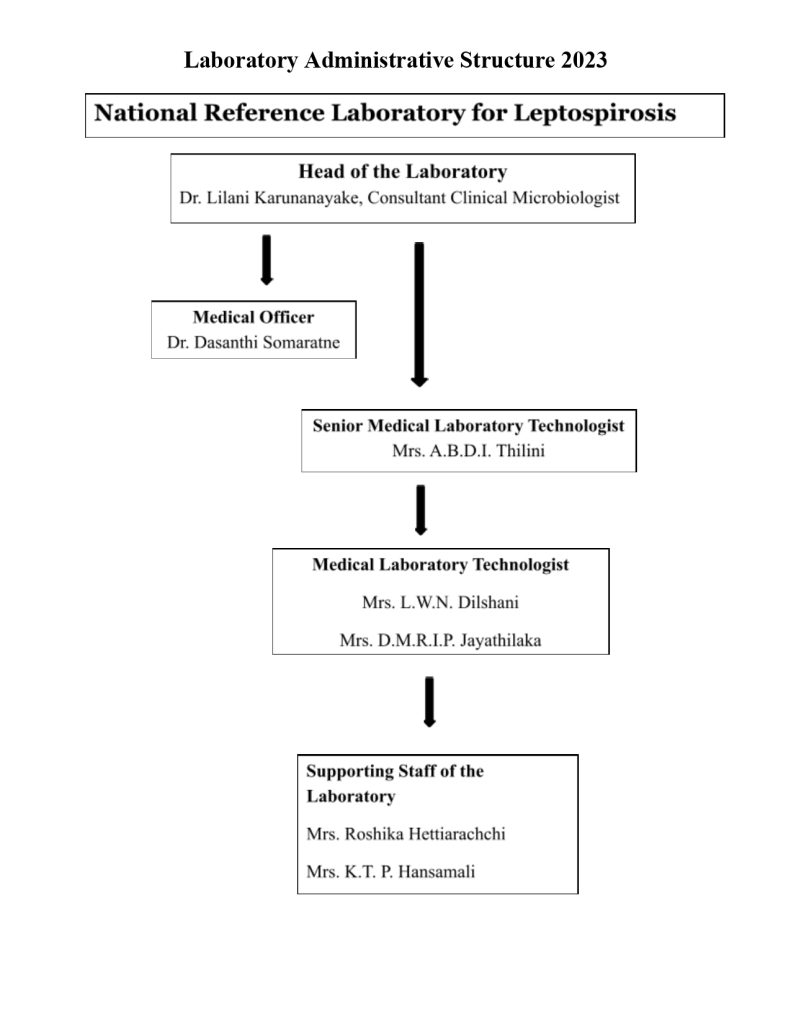
National Reference Laboratory for Leptospirosis
Head of Laboratory
Dr. Lilani Karunanayake
Consultant Clinical Microbiologist
HISTORY
Eight new reference Leptospira serovars from human and animals have been added from Sri Lanka to the world literature (gem, alice, weerasinghe, ratnapura, ceylonica, jeyaweera, lanka and animal spp.) In 1971, Dr. Nityananda identified many different serotypes and their reservoir hosts in Sri Lanka. The findings suggested the existence of a diversity of serotypes maintained by different maintenance hosts such as rodents, domestic farm animals and dogs [K. Nithyananda et.al.,‘Leptospirosis in Ceylon]. In 1962, a serological survey of occupational groups showed rice field workers, sewer workers, workers in coconut plantations and desiccated coconut mills, sugar cane workers, abattoir workers, fish market workers and river bathers were as at risk of leptospirosis.
Heads of National Reference Laboratory for Leptospirosis
1953 – Dr. K. Nityananda, Consultant Bacteriologist
1970’s – Dr. M. Atapattu, Consultant Microbiologist
2000 – Dr. Philomina Chandrasiri, Consultant Clinical Microbiologist
2003 – Dr. Praneetha Somarathne, Consultant Clinical Microbiologist
2011 to date – Dr. Lilani Karunanayake, Consultant Clinical Microbiologist

Guideline for Collection and Transport of Specimens for the Diagnosis of Leptospirosis to Medical Research Institute General Circular No. 01-51/2018
Presently available tests:
- Microscopic Agglutination Test (MAT) Pathogenic Panel
- Leptospira detection by qPCR from blood and urine
- Blood culture
- Urine / CSF Microscop





